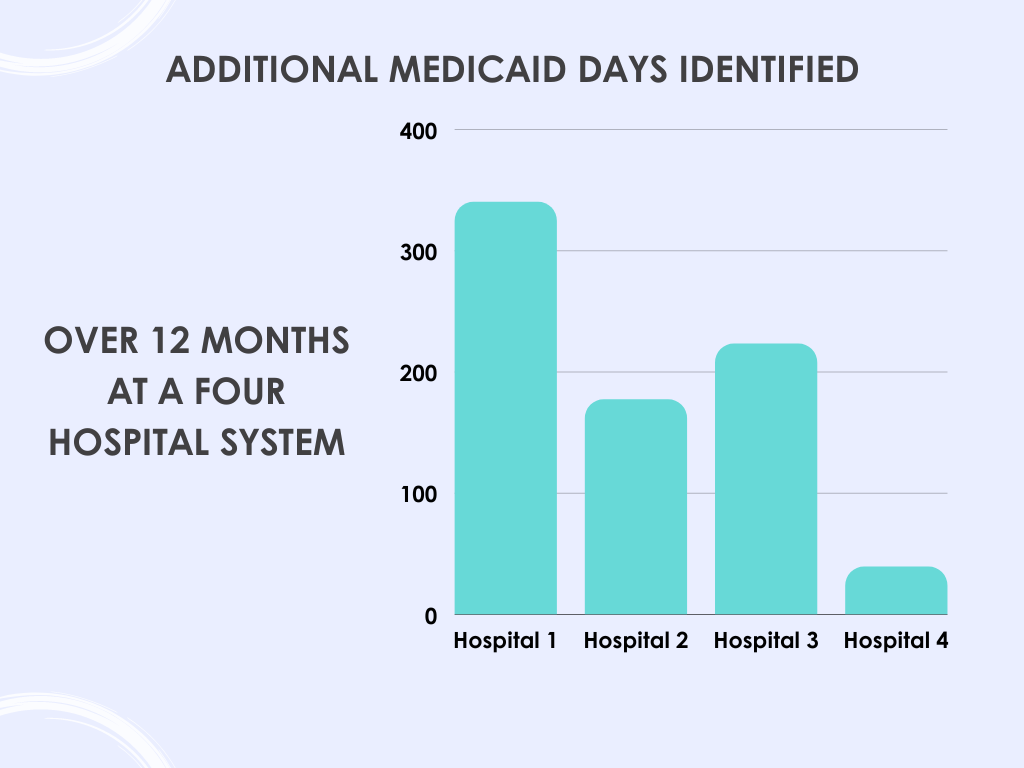
Real World Example
Hospitals at risk of losing 340B eligibility and/or DSH status have experienced significant increases in Medicaid Days after engaging with Nemadji's Eligibility Detection solution.
Hospitals have multiple processes in place throughout all the stages of their revenue cycle to identify insurance coverage.
Even so, things still fall through the cracks.
By continuously screening accounts for eligibility, Nemadji is is able to identify and verify previously unknown, billable coverage. In some cases, coverage could not have been detected at an earlier point in the process.
As a result, additional insurance payments are collected, Medicaid inpatient days are increased, fewer accounts are written off or sent to bad debt and patients are left with correct financial responsibility.
For some, the identification of additional Medicaid days is critical in maintaining or obtaining DSH and/or 340B eligibility.
In just one year, a four hospital system was able to identify and add a total of 779 Medicaid days through our partnership.